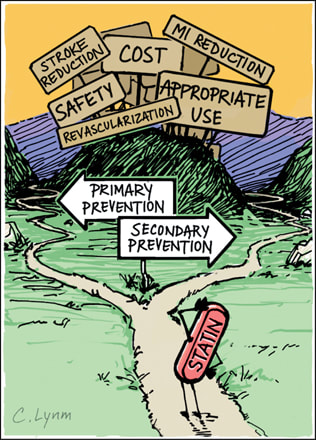
On a daily basis I encounter patients who refuse to take statin medications. The Internet provides so much information and misinformation that mythologies abound and it is very hard to sift through what is meaningful and what is not. This blog contains a lot of information: it is everything you wish to know or don't want to know about the importance of statin therapy.
The class of drugs known as statins was discovered by Dr. Akira Endo at Sankyo in Japan in the early 1970’s.
It inhibits the enzyme 3-hydroxy-methylglutaryl-coenzyme A (HMG-CoA) reductase. Merck&Co. launched the first statin made available to the public, lovastatin (Mevacor) in 1987.
Lovastatin and the other statins that followed have resulted in a substantial reduction in virtually all clinical manifestations of atherosclerotic vascular disease, including coronary events, strokes, and revascularization procedures, and have prolonged the lives of millions of people.
Of the 6 most commonly used statins, 3 are derived from fungi (lovastatin, simvastatin, and pravastatin, and 3 are synthetic (fluvastatin, atorvastatin, and rosuvastatin). As mentioned, statins block or “inhibit” HMG-CoA in the liver and this blocks a protein called mevalonate,
which then suppresses the manufacture of cholesterol; the stronger the statin, the more mevalonate that is inhibited. Additionally, the more this occurs (with the stronger statins) more LDL receptors are manufactured in the liver cell to go to the cell surface to remove circulating LDL into the hepatocyte (liver cell) and degrade the LDL into bile acid.
Statins have a significant lipid lowering effect and have significantly lessened the event rates of coronary artery and other arterial diseases. It must be noted that though 1/3 to 1/2 of those who take statins have benefit in outcome, 1/2 to 2/3’s do not.
Though the reduction of cholesterol and LDL levels are proposed as the primary principle for arterial protection, it is not the sole mechanism for benefit. There are several actions that are independent of cholesterol lowering:
1)Statins improve inflammation in the artery wall and can improve features associated with plaque stability.
2)Blood C-reactive protein (CRP), a marker of inflammation is reduced by statins independently of the amount of cholesterol lowering.
3)Statins improve endothelial function rapidly, before any appreciable reduction in serum cholesterol can be detected. (The endothelium is the lining into the artery wall).
4)Statins reverse endothelial dysfunction in young smokers with normal LDL levels.
5)Regression of coronary atherosclerosis, and improvement in clinical outcomes with intensive statin therapy are related equally to reduction of CRP and other inflammatory markers as well as LDL cholesterol regulation.
If statins offer benefits that are independent of cholesterol lowering, how does this occur?
There are a group of complicated protein interactions (the rho proteins), that influence cellular membrane metabolism. This process triggers much of the atherosclerotic process: reduction of nitric oxide, acceleration of vascular inflammation, increased levels of inflammatory proteins, increased vascular smooth muscle proliferation, increased levels of thrombotic (clotting) factors. (Plus many more very complex cellular and biochemical interactions).
Statins interact with and reduce these Rho proteins . This produces a decrease or even a complete reversal of most of the atherosclerotic cellular processes listed previously. This is a very important arena of science and clinical research.
Lipid Effects:
The evidence that lowering LDL cholesterol reduces cardiovascular events is very strong!:
Statins are the preferred first line treatment of choice for coronary disease risk reduction within the context of pharmacological therapy. The concept of “lower is better” is supported by a lot of data.
The statins differ in their LDL lowering capability. This was demonstrated in the STELLAR trial (Statin Therapies for Elevated Lipid Levels Compared Across Doses to Rosuvastatin). This was a randomized, parallel -group, open label, comparator-controlled trial of 2431 hypercholesterolemia adults to compare lipid changes after 6 weeks for all of the statins and doses tested: Rosuvastatin lowered LDL cholesterol across its 10 to 40 mg dose range by 46% to 55%, compared with 37% to 51% for atorvastatin 10 to 80 mg dose range, 28% to 46% for simvastatin 10 to 80 mg dose range and 20% to 30% for the pravastatin 10 to 40 mg dose range. This LDL lowering effect is reflected in their ability to attain the earlier National Cholesterol Education Program Adult Treatment Panel 111 (NCEP ATP111) LDL goals.
Again, from STELLAR, the percentage of coronary heart disease patients who achieved treatment goal of less than 100 mg/dl with Rosuvastatin 10 mg, Atorvastatin 20 mg, Simvastatin 40 mg and Pravastatin 40 mg were 55%, 43%, 31% and 11% respectively.
Another example of statin effectiveness to achieve LDL lowering to less than 100 mg/dl was studied with Rosuvastatin in a group of patients with very high LDL levels from 190 to 240 mg/dl (this group has heterozygous familial hypercholesterolemia). Rosuvastatin 10 mg lowered LDL to less than 100 in 37% of patients, and 20 mg lowered LDL to less than 100 in 66%.
Statins also lower triglycerides, generally in the range of 15 to 30%, also in relation to the strength of the statin in lowering LDL. Generally, the greater the baseline triglyceride , the greater the lowering. Patients who have triglycerides of greater than 200 tend to have a more aggressive lipid atherosclerotic pattern. This goes along with metabolic syndrome which is a pre-diabetes picture: High levels of triglycerides, low levels of HDL, increased VLDL particles, and LDL particles that are smaller, more dense, and greater in number which are more aggressive in the atherosclerotic profile.
Statins have been shown to be effective in improving all of these parameters. By their very mechanism of action, statins remove VLDL and LDL particles from the circulation. There is not only reduction in concentration of particle number of LDL and VLDL but also a preferential removal of smaller dense LDL particles. In one study, atorvastatin removed 44% of small dense LDL particles and 10% of larger particles and 31% of all LDL particles. By contrast, niacin, a drug used for patients with this more aggressive atherosclerotic profile, shifted small LDL particles to larger ones and reduced particle number by 14%. Niacin does have a beneficial effect on increasing HDL levels by 10% to 15%. Rosuvastatin may raise HDL to 8% to 10%.
Impact on Morbidity and Mortality
Statins have been evaluated in more than 100,000 individuals participating in randomized, controlled clinical event end point trials: over 18 large population studies, both primary risk prevention studies (no coronary or arterial event has occurred yet) and also secondary risk prevention studies ( the event has occurred, and we’re trying to prevent the next one).
The conclusion for all of these studies is that all outcomes of atherosclerotic vascular disease is reduced with statin therapy including coronary artery disease death, non-fatal MI, coronary revascularization, acute coronary syndrome, unstable angina, stroke, peripheral vascular disease, cardiac arrest, and heart failure.
Reductions in total mortality have been specifically documented in 4S, LIPID (Long Term Intervention with Pravastatin the Ischemic Heart Disease), and HPS (Heart Protection Study).
Several of the Primary Prevention studies include:
1.the ALLHAT Study with 10,335 adults double blinded to placebo or Pravastatin 40 mg/day. There was an average of LDL lowering of 17% and a lowering of coronary or stroke events by 9% over 4.8 years.
2.the ALERT study with 2100 adults on placebo or Fluvastatin 40 mg/day showed an average lowering of LDL of 32% and a lowering of coronary events of 35%. The average reduction of cardiac death, nonfatal MI and revascularization was 17%. Followup was 5.1 years.
3.the ASCOT trial included 14,350 adults treated with placebo or Atorvastatin 10 mg. the LDL average lowering was 35% and reduction in CHD events was 31% with followup of 3.3 years.
4.SPARCL with 4731 adults treated with placebo or Atorvastatin 80 mg had LDL lowering of 45% and a reduction of coronary events of 35% over 4.9 years.
5.WOSCOPS trial with 6595 men, treated with placebo or Pravastatin 40 mg daily. LDL lowering was averaged at 26% and coronary events lowered by 31% over 4.9 years.
6.AFCAPS/TEXCAPS study had 66065 adults treated with placebo or Lovastatin 20 to 40 mg day . LDL lowering averaged 25%, and coronary event lowering averaged 40% over 5.2 years.
Secondary Prevention studies are studies where a coronary vascular event has already occurred. Some of these studies are:
1.4S: 4444 adults treated with placebo or Simvastatin 40 mg daily. LDL lowering was 35%, coronary event reduction was 34% over 5.4 years.
2.LIPID: 9014 adults treated with placebo or Pravastatin 40 mg. LDL lowering was 25% and coronary event reduction was 24% over 6.1 years.
3.CARE: 4159 adults treated with placebo or Pravastatin 40 mg. LDL lowering was 32% and coronary event reduction was 24% over 5 years.
4.HPS: 20,536 adults treated with placebo or Simvastatin 40 mg. LDL lowering was 32% and coronary event reduction was 27% over 4.9 years.
5.TNT: 10,000 adults treated with placebo, or Atorvastatin 10 mg vs. Atorvastatin 80 mg. Further drop in LDL lowering of 24% and a further reduction in coronary events of 22% over 4.9 years.
It is important to comment that all of the above dramatic percentage drops in LDL lowering and disease event rates are not percentages based on the total number of patients. These reductions are called relative risk reductions and an example would be the following:
Of 10,000 patients, 200 patients taking placebo had a cardiovascular event, and 100 patients taking statin had a cardiovascular event. That would represent a 50% reduction based on RELATIVE RISK criteria which in clinical double blind randomized studies MUST achieve statistical significance by at least 0.05%. This is based on the numbers in the study, the percentage of people responding, and the length of time of the study. It would be a mistake to think that in a 10,000 person study, 7000 had coronary events on placebo and 3000 had events on statin. That is something that never occurs in these types of studies.
The statins are effective at reducing cardiovascular event rates in patients with existing vascular disease (secondary prevention) as well as those with only risk factors (primary prevention). Statins are equally effective in reducing risk and events in men and in women, irrespective of age. Statins are effective in reducing events in diabetic patients. Patients with diabetes or metabolic syndrome often have atherogenic dyslipidemia with only modestly increased LDL. In spite of this, statins are excellent treatments of choice in these patients because they effectively reduce small dense LDL particles, cholesterol-enriched remnant particles and overall particle number as discussed above. The Collaborative Atorvastatin Diabetes Study (CARDS) specifically studied type 2 diabetic patients and reported a 37% relative event reduction which was so robust that the trial was stopped prematurely.
In 2012, there was a departure from the original NCEP ATP111 recommendation of driving LDL to less than 100 in intermediate risk patients and to less than 70 in higher risk patients. Though the National Lipid Association and several European cardiovascular societies have maintained this recommendation, the American College of Cardiology presented a new recommendation of achieving a 30% lowering of LDL from baseline in intermediate risk patients and a greater than 50% reduction in the higher risk groups. Though there is considerable debate amongst the various professional groups, the primary caveat is the importance of LDL lowering through diet and exercise programs and then utilizing pharmacologic tools with statins as the primary recommendation.
OTHER ISSUES:
Alzheimer’s Disease.
Alzheimer’s Disease is a neurodegenerative disorder that leads to cognitive decline and neuropsychiatric symptoms and diffuse structural abnormalities in the brain. It is characterized by the deposition of amyloid plaques and neural fiber tangles that may be related to cholesterol synthesis.
Evidence that links cholesterol and Alzheimer’s Disease has come from observational studies. It has been observed that an elevated cholesterol level in mid-life increases the risk of Alzheimer’s Disease to 2 to 3 fold in later life. Conversely it has been observed that people who take statins and other lipid-lowering agents have a 60% to 75% reduction in the future risk of Alzheimer’s Disease.
Liver.
Elevation of liver enzyme blood tests to greater than 3 times normal with statin therapy are rare. In one meta analysis of 74,102 patients the incidence of this was 1.4% in statin treated patients and 1.1% in placebo control patients. It appears to be more related with the intensity of the statin dose rather than the degree of LDL lowering. It also tends to be transient. In an analysis of 180,000 people it was reported that 300 in 90,000 treated with a statin had elevations of 3 times normal. Of the 300, only 110 had consecutive elevations with another repeated blood test.
The incidence of actual liver failure is extremely rare. In the FDA Adverse Event Reporting System (AERS), it was calculated that there was 1 case in 1.4 million patient-treatment-years. In fact the incidence of 1 case per million is the same in patients taking a statin as well as with people NOT taking a statin.
In the context of a 3 fold increase in liver enzyme blood tests it is considered prudent to interrupt statin therapy for a brief period of time and reassess lab values and then resume therapy. It is recommended that the clinician evaluate clinical symptoms and signs of liver dysfunction ( malaise, fatigue, loss of appetite, weight loss, jaundice). It the blood tests normalize or if the blood tests are only mildly elevated, then the statin therapy may be resumed, or in the latter case, not interrupted.
The position of the National Lipid Association is that interruption of statins with mild elevation of liver blood tests (<3 times normal) to avoid a very remote risk of liver failure, the patient will be exposed to a disproportionally higher risk for cardiovascular events.
Patients with nonalcoholic fatty liver disease have a significantly increased cardiovascular risk and are candidates for statin therapy. Statins are actually safe in these patients. Statins do not further elevate baseline liver enzyme abnormalities, and in fact may actually improve liver function.
Muscle.
The 2 more serious muscle problems are myopathy (muscle discomfort, pain, weakness, with an elevation of creatine kinase (CK) to greater than 10 times upper limit of normal, and rhabdomyolysis ( the above with associated kidney failure and higher risk of death).
These serious muscle-related adverse effects are rare. In an analysis of 21 randomized clinical trials with 180,000 person-years of followup on statin therapy or placebo, myopathy occurred in 5 patients per 100,000 person-years, and rhabdomyolysis in 1.6 patients per 100,000 person-years. The AERS database reported a rate of 0.3 to 2.2 cases of myopathy and 0.3 to 13.5 cases of rhabdomyolysis per 1 million statin prescriptions.
Muscle toxicity with statins is a class effect but there appears to be a difference between weaker and stronger statins. Pravastatin was not associated with a case of rhabdomyolysis in 19,768 people studied for 5 years. Simvastatin produced rhabdomyolysis in 0.1% of 2265 patients on 80 mg in the A to Z trial.
The more common adverse effect of statins is myalgia, which is muscle soreness, pain, or weakness. This is not associated with the above serious complications of myopathy or rhadbomyolisis. The incidence of myalgia varies between 5% to 15% in the literature. There tends to be some misinformation as to the accuracy because there is often confusion about what constitutes statin related myalgia, versus a localized sore muscle or joint, related to activity or arthritis. Reports of myalgia with statins in clinical trials are the same as, or only slightly more than, those reported in patients receiving placebo. However, this complaint is the most common reason for patients to discontinue therapy.
A specific gene has been discovered that affects liver uptake of statins. This gene (rs4363657) occurs in about 15% of the population. With this gene, statins would not be taken up as freely into liver cells thus elevating statin blood levels. Also higher statin doses, and drug interactions may also increase the statin blood level and thereby increase the risk of muscle achiness.
Some investigators have related the cause of myalgia and myotoxicity to a drop in ubiquinone levels. This is also known as coenzyme Q10 (CoQ10). Ubiquinone plays a role in cellular energy and cell membrane activity. It is carried in LDL particles and thus, with lowering of LDL levels there is also a lowering of CoQ10 levels. There is some conflicting data as to the measurement of CoQ10 levels in muscle cells, and the lowering effect related to dosage of statin. There have been conflicting results on the benefits of giving CoQ10 to patients to prevent or to treat muscle-related symptoms. In one study that used high doses of lovastatin, supplementation with CoQ10 240 mg daily did not reduce the frequency of myalgia compared to those not receiving it. In another study, statin-taking patients who had myalgia had their pain assessed on a 10 point grid. Those given 100 mg daily CoQ10 had reduction of 5 to 3 with the addition of this: Somewhat equivocal!
However, there are no known risks associated with taking CoQ10. Giving patients CoQ10 may be tried in patients who develop myalgia and cannot otherwise tolerate statin therapy.
The clinician should also be aware of anything that can elevate statin blood level. This would include higher dosage, older age, frailty, female gender, renal insufficiency, hepatic dysfunction, hypothyroidism, and use of other pharmaceutical agents that have interaction with statins.
I’ve addressed before the complexity of the disease called “Atheroscelerosis”. I’ve discussed how it can smolder and develop over decades and then how it can suddenly erupt: with a ruptured plaque causing an acute coronary event.
In preventive cardiology, we are committed to impacting this mysterious and complicated process. There are 3 objectives: first is to try to slow down the atherosclerotic process, second is to stop it, and third is to reverse it.
When people are unable or unwilling to engage in the science of pharmacology, they are removing very important ammunition to engage this unrelenting disease. Obviously there are many facets that are called into play: appropriate nutrition, exercise, weight management, avoidance of diabetes, hypertension and smoking. Most people know what to do as regards these behavioral issues, how many are successful in conquering these issues? I’ve learned that optimization of your body’s hormones plays an exceptional role as well, but when overt bias exists that is oppositional to the gift that the science of pharmacology has given us, why would you put yourself in a position whereby you are not giving yourself the best opportunities to counter this difficult and unpredictable disease?
The bibliography to the above essay is obviously very extensive and is not listed here. However, much of the essay was synthesized from the chapter on Statins, written by James McKenney, Peter Ganz, Barbara Wiggins, and Joseph Saseen in the textbook of Clinical Lipidology, edited by Christie M. Ballantyne.
 RSS Feed
RSS Feed