|
I had two patients send me this article from the New York Times written by Dr. Haider Warraich, M.D., who is a cardiologist. I found it interesting and wanted to share it with you. Click the button below!
3 Comments
As I’ve previously mentioned in earlier essays, coronary artery disease caused by the underlying disease of ATHEROSCLEROSIS is by far and away the Number One cause of dying per year in the United States. Death occurs most commonly by Ventricular Fibrillation with over 400,000 people dying suddenly, most of them with underlying coronary artery disease. Another million people will have heart attacks, which may or may not kill them, and they may also end up with Congestive Heart Failure, which can be treated, but can also lead to significant incapacity and death. (I refer you back to my earlier essay on HEART DISEASE which explains the underlying disease process of Atherosclerosis and how it can suddenly create a sudden event causing a Heart Attack (Myocardial Infarction). In fact, most of our efforts as Cardiologists, are based around, not only taking care of these emergency- based problems, but also trying to thwart the progress and ongoing development of Atherosclerosis so that it doesn’t cross over to the clinical expression of coronary artery disease). So, this topic, is Public Health Enemy Number One! An actual heart attack is referred to in medical language as a Myocardial Infarction, (or MI), and is divided into 2 subtypes: Acute STEMI (ST Segment Elevation Myocardial Infarction), or NON-STEMI.
The time sequence of entry into the hospital to the moment the artery is “ballooned” open is measured and must be initially under 90 minutes, and is now expected to be under 60 minutes. This is a national health policy and something every hospital is assessed on. We at Hoag, on a quarterly basis, are usually at the 100% level! The reason why this time interval is so important, is because “Time Saves Heart Muscle”. In other words, when a total blockage of an artery occurs, there is no flow of blood going down the artery and the area of heart muscle cells that are fed oxygen and nutrients are suddenly deprived. As time goes by, heart cells start to get injured and begin to die off. The longer the time, the more degree of injury and eventual cell death. If the blockage is high up towards the source of the artery, the greater the area of heart muscle at risk. The farther down the blockage is, the area would become relatively smaller, so the damage to the heart may not be as big an area of injury and cell death. NON-STEMI A non-STEMI MI, is also known as an Acute Coronary Syndrome (ACS). The presentation of the patient may be the same with chest pain and other symptoms, but the EKG does not show the ST segment elevation. It will show other EKG changes, but the bottom line is that this type of presentation does not usually suggest an acute blockage of a specific artery, and is not considered as being the same type of immediate emergency as the acute STEMI MI is. In this regard, we would usually observe and stabilize the patient first with a variety of heart medications. Certain tests may follow including further EKG’s, lab tests, echocardiogram and nuclear imaging tests, or special CT angiograms, and if necessary, a heart catheterization study to do an angiogram. This may lead to further intervention with angioplasty and stenting, or even bypass surgery... or none of the above, and the patient is taken care of with the use of long-term medications. The reason for this is that the artery in this context is not usually completely blocked, and there may be various degrees of limited flow going through, and there may also be more complex coronary issues involving narrowing of other arteries. Let me mention the immense skill, training, knowledge, and trouble-shooting capabilities of the Interventional Cardiologist, and the Cath Lab Team. Firstly, because of the urgency to get to the hospital as fast as possible to “Get That Artery Open”, is a whole different story when an emergency occurs during the day , during regular “business hours” versus evening, night time, holidays and weekends. The stress level is very high. The On-Call Phone is always at your side, even if you’re going to the bathroom, or having a shower, or you’re trying to sleep in the middle of the night. When the call comes, you go, and you go as quickly as you can. The doctor and the team are walking into a completely unknown situation, each and every time. Some of the issues are: how much time went by before the patient even showed up? What is the clinical stability of the patient? What is the intensity of their pain? What is the extent of the damage and the degree of heart failure? Is the blood pressure stable, or are they in cardiogenic shock? Are they having arrhythmias? Which ones? Are they having cardiac arrest and ventricular fibrillation? Do they need balloon pumps and other heart augmentation devices? (On many occasions we don’t even know who the patient is, or what the story was.) Where is the culprit blockage? Which vessel? How complex is it? Does it involve one artery, or is it at a bifurcation of 2 arteries? How long is it? How many other narrowings are present? Can we get the wire passed? Can we get it through the blockage? How do we prevent the wire from perforating of dissecting the artery which can lead to death? How can we stabilize the heart rhythm when recurrent cardiac arrest keeps continuing? Now I bet you are wondering WHAT IS AN ANGIOGRAM, ANGIOPLASTY, AND STENT? Click on the link provided to watch this video at your convenience (FYI- Skip the Ads)!. It does a good job of demonstrating what we do as cardiologists in the cath lab. www.youtube.com/watch?v=N7nghr9TpSU Here’s a Little Joke: A mechanic is working on the engine of a cardiologist’s nice car. He had to change a valve. It took several hours. He was complaining to the doctor that he only made $75 an hour, and given the car he was driving, the doctor must obviously make more an hour than he did. Whereupon, the cardiologist said, yes I understand, but when I work on an engine, it’s running! (This is obviously an old joke because in this era, I think plumbers and mechanics are now actually earning more per hour than we are! LOL) ☹ WHAT YOU NEED TO UNDERSTAND ABOUT CORONARY ARTERY DISEASE: Coronary artery disease does not necessarily always unfold with gradual plaque buildup to the point of blood flow compromise and then the artery finally blocks off. This does happen to many people and their presentation is often one of recurrent exertional ANGINA chest discomfort, and/ or the stress tests and echoes and scans will show abnormalities that will lead to an angiogram and then stenting or bypass surgery. These plaques that compromise coronary blood flow are fixed, rigid, and calcified. However, the majority of people having an acute Myocardial Infarction do not have these very high grade obstructive narrowings causing that specific event. These people have plaques that are not fixed, rigid, and calcified. They may not be impairing coronary blood flow at all. They may narrow the artery by 20% to 50% which is not sufficient to cause flow impairment. BUT they are VULNERABLE and INFLAMED and SOFT, and may become UNSTABLE. I compare these plaques to “Creme Brûlée” because they have a “hard cap” filled with cholesterol and inflammatory products and they can unexpectedly and unpredictably FRACTURE or RUPTURE and when this occurs, the artery is acutely blocked and heart attack has begun. Here are 2 stories where 2 people survived: One who got to the hospital quickly, and had restoration of blood flow through a blocked artery, and his heart function got back to normal, and he was given a new lease on life. The other, did not get to the hospital quickly because he didn’t even know he was having a heart attack. Unfortunately, he has been left with a permanently damaged heart. However, with good medical care, he is still alive and doing pretty well, and he realizes how lucky he has been. Both of these patients had “ruptured plaque”. Patient # 1 is a 66-year-old man. He considers himself to be in very good shape and goes to the gym a lot and does a lot of weight lifting. He also rides his bicycle several times a week from the Newport Pier to the Huntington Beach Pier. However, he was noticing a sharp and aching pain to his left chest muscle area when he would lift himself into his bed. (It is a bed that is fairly high up off the ground, so he has to face the bed backwards, and use his arms to lift himself up). He also noticed the same pain when he moved his arms across his chest. He did not have any chest discomfort when working out, or when riding his bicycle. I felt that he was having pain from strained pectoral chest muscles, from his weight lifting, and provoking it with his various movements and body positions. He did not have any pain or discomfort that sounded like angina when he was exerting himself. However, this patient has risk factors including diabetes and high cholesterol numbers. He was not paying attention to his diet, and he was not on the correct doses of medications- when he took them. I referred him to a different endocrinologist, and I changed his cholesterol medications to get his levels into the correct range. I had him do a treadmill, and he exerted well, without discomfort, however, he did have non diagnostic stress test with non-specific abnormalities on the EKG. Therefore, we went on with a more precise study, called a nuclear imaging study. All of his heart testing was perfectly normal. Interestingly, right after he finished his study (which was normal showing no perfusion abnormalities that would indicate blockage), he went to have lunch with some friends. While eating he had the sudden onset of a heavy, crushing, quite severe central chest discomfort, associated with sweating. He never had anything like this before. His friends did not ignore this and drove him immediately to the hospital. His EKG showed an Acute STEMI. He was taken immediately to the Cath Lab and the angiogram showed a total blockage of his major left coronary artery (left anterior descending artery). Though it may sound straight forward, the artery was successfully opened with a very good door to balloon time and it was successfully stented. He went home 2 days later, and went on to full recovery (His initial left ventricular function was diminished due to the acute injury, but when we repeated his echocardiogram 6 weeks later, it was perfectly normal). Though he initially blamed us for missing something, he demonstrated no insight into the fact that he never took his medications in a committed way and the control of his diabetes and cholesterol was, in fact, quite inadequate. He also had a hard time understanding the concept of plaque rupture! But many people have trouble understanding this. Patient # 1 has not had a recurrence. He is still exercising, and is now on correct medical management involving good diabetes treatment, cholesterol numbers are very good with LDL driven well below 70, and he is on appropriate combination of anti-platelet medications (blood thinners). Patient # 2 is a 70-year-old man. He was sent over to my office by his family doctor because he was short of breath, weak, tired, loss of appetite and energy, and he was in atrial fibrillation but was not at all aware of his heart beat. His heart rate was moving along appropriately, not too fast. His EKG was very abnormal, showing an anterior wall Myocardial Infarction, though he wasn’t aware that he had ever had a heart attack! However, on questioning, he recollected that 8 days before, he was walking through the airport and he had upper mid abdominal and upper left abdominal pain that was quite severe. He actually went to a local Emergency Room and was found to have kidney stones. Because it was felt that the pain he was having was due to the kidney stones, no heart work up was done. I explained to him that the EKG in our office showed he had had a heart attack, and that he was in CONGESTIVE HEART FAILURE, which was completely astonishing to him. He came back the next day for an echocardiogram which confirmed the story: profound weakening of the left ventricle! We measure the performance of the left ventricle which is called the EJECTION FRACTION (EF). A normal EF is from 50% to 75%. His EF was only 16%! This means he was really in bad shape with very, very weak heart performance, and also with significant leakage of the Mitral Valve. So he now had a completed event with full and terrible damage done to his heart. He was now in severe Congestive Heart Failure, by which he could die, and he was also at significantly increased risk of dying of SUDDEN DEATH by Ventricular Fibrillation. He was immediately admitted to the hospital and started on all the appropriate medications for correction of heart failure, protection of life-threatening arrhythmias, as well as treatment for his atrial fibrillation, and appropriate lowering of his cholesterol. He also had a heart catheterization (angiogram), and interestingly, we found that he had a single blockage of the left anterior descending artery (LAD) which had spontaneously reopened with what was now a 50% to 60% narrowing, so he did not need a stent. What apparently happened, was that he had a plaque rupture blocking the artery causing the heart attack, likely when he was going through the airport, and by good luck, at some point the artery re-opened! However, not before very serious damage was done to his left ventricular function. He went home on all of his new medications and he was given a LIFE-VEST that he had to wear all the time because of the increased risk of having a sudden cardiac arrest. LIFE VEST AND ICD The Life-Vest is an external defibrillator that you wear for several weeks before we are allowed to put in an Implantable Cardioverter Defibrillator (ICD). In some people we will see an improvement in heart function over a 6-week period, so they do not require a permanent ICD, whereas other people continue to have problems with weak hearts and heart failure and they require an ICD for hopeful prevention of sudden death, and in some cases further therapy for correction of heart failure. The ICD detects life-threatening arrhythmia and will shock the patient hopefully back to normal rhythm if the arrhythmia reaches predetermined thresholds that indicate a life-threatening situation. (The topic of Sudden Death and the development of the Implantable Cardioverter Defibrillator (ICD) is an entirely separate essay as is the topic of Congestive Heart Failure) He continued to have problems with breathing, exhaustion, weakness and his heart function over this period did not improve, so he, in fact, received a very special device which is a Bi-Ventricular ICD. This ICD not only treats and terminates life threatening arrhythmias such as Ventricular Tachycardia, and Ventricular Fibrillation, but also paces the heart in both left and right ventricles, and may improve heart contractility and improve the clinical problem of congestive heart failure. Two years later, he is alive and doing pretty well. He is able to walk now without shortness of breath, and in fact, says he feels pretty well. His heart function has improved but not up to normal range. He still has some weakness of his heart, but his life quality is quite good and he is extremely grateful. CONCLUSION: Each patient who has a heart attack is unique and each one is an individual human story. I have given you a picture of the enormity of what we face with CORONARY ARTERY DISEASE and MYOCARDIAL INFARCTION. Heart Attack can be a devastating HEALTH ATTACK and can completely change your life or take your life. Please refer back to my earlier essays on Heart Disease, Lifestyle, Hypertension, and Statins. These essays will explore many of the topics touched upon in this essay, and will give you further insight into the importance of what we do for disease prevention, as well as provide encouragement for good health. Most of you are aware that for many years, I have been interested in practicing preventive cardiology. This dates back to over 10 years ago when I got board certified in Clinical Lipidology. Thus, in addition to taking care of many people with active and serious heart problems, I have also worked hard in trying to prevent these problems from happening, and to give people the potential of living better lives.
About 4 years ago, I became increasingly interested in the medicine of hormones and how they work in your body, particularly as we age: the question being, “How can we maximize our potential as human beings, in terms of good health, vigor, energy, and mindfulness, as we age?” In 2017 I studied extensively and participated in 4 courses, over a total of 100 hours of course material, on the subject of “Mastering the Protocols for Optimization of Hormone Replacement Therapy”, taught by Dr. Neal Rouzier: a fascinating learning experience. I would like to present here, an overview of the concepts of natural hormone replacement therapy. I won’t be discussing specific hormone literature, as I have previously done with testosterone, and also vitamin D. There will be further essays written on estrogen and progesterone, and thyroid at later times. This essay will be predominantly a series of passages from Dr. Rouzier’s booklet of “Bioidentical Hormone Replacement Therapy” and should give you very good insight into what this is all about. “Conventional medicine has always held the belief that aging is inevitable and that the progressive deterioration that occurs in our adult years cannot be altered. This is simply not true. We have also been lead to believe that the diseases of aging, such as heart disease, stroke, cancer, and senility, are all a part of the normal aging process. The downward spiral of physical and mental decline that we have come to accept as a natural part of growing older is becoming recognized as somewhat controllable and preventable. The most effective solution of any disease process is prevention of that disease. We are now in an era where mainstream medicine is now focusing on slowing down the aging process with the science of genomics, telomeric application and optimal hormonal supplementation. Research is showing that maintaining our hormone levels in a youthful state can help prevent the debility and illness that accompany the aging process. Hopefully this will lead to increased longevity by preventing the illnesses that usually lead to our demise, and more importantly is the possibility that our quality of life in our later years may be significantly enhanced.” “Over the last 50 years research in the fields of endocrinology and immunology has improved our knowledge as to how and why we age. The rate and incidence of disease formation as well as the rate of aging are partially controlled by our endocrine and immune systems. The endocrine system regulates our body’s temperature, reproduction, growth, aging and immune system. Communication between the nervous system, the endocrine system and the immune system makes it possible for us to adapt and survive in our environment. It is through hormones that these systems interact with each other. Hormones are molecules that are released into the blood stream and exert biochemical effects on distant organs and cells. Hormones can affect every cell in the body by activating receptor sites on the cell and thereby cause an internal activation of protein synthesis and activity. The hormone’s effect is determined by a specific receptor site on the target cell. Hormones exert different actions on different cell types in different tissues. A decrease in the production of hormones begins in middle age and continues to diminish in a linear fashion until old age.” “Hormones are either proteins or derivative of cholesterol. These molecules are manufactured in endocrine glands, which include the adrenal glands, the testes, ovaries, pancreas, thyroid, pituitary gland and pineal gland. When there is degeneration and aging of the organs, the levels of hormones diminish. In addition, the specific receptor sites on the cells tend to change and deplete and become less interactive with hormones as they once were in our younger years. Whether the problem is low hormone levels or hormone resistance, the solution is optimal hormone replacement.” “Whatever the cause may be, any decrease in stimulation of the receptor site will result in a decrease in stimulation of the cell, decrease in cellular repair, decrease in protein synthesis, inability of the cell to regenerate and a gradual destruction of the cell. This is what occurs with age. A deficiency of hormones will therefore result in an imbalance in this very precise, self-regulating system.” “For many years, medicine has recognized the health benefits of replacing these waning hormones. For most physicians, synthetic hormones were the only option. Now it is possible to produce natural hormones that in every way match those produced by the body. Most hormones can be derived from plants, such as soy and yams. What is most important is that the end product is a molecule identical to the hormone molecule found naturally in the body. This applies to all hormones—thyroid, estrogen, progesterone, testosterone, DHEA. We have come to understand that synthetic hormones, which are chemically different that those naturally found in the body, can cause a whole host of side effects and even cancer. it does not make sense whatsoever to replenish with chemically different hormones when bio-identical hormones, to which our bodies are accustomed, are available.” “You might ask, ‘if there are hormones available that are natural to my body, who do doctors prescribe synthetic hormones?’ The explanation involves the powerful pharmaceutical industry in the United States, politics and economics. The molecule of the natural hormone is identical in structure to the hormone naturally found in the body. Pharmaceutical companies cannot patent natural or bioidentical compounds. However, they can patent chemically different molecules that are highly profitable. A patent will guarantee that a pharmaceutical company will have an exclusive right to manufacture and profit from their product. After the tremendous monetary investment that goes into developing and studying a pharmaceutical product, it is logical that the pharmaceutical companies would want their investment protected with an exclusive, patented product. Therefore there is little research and minimal marketing of natural hormones.” “A large part of marketing a drug involves the education and instruction of a physician on how and when to prescribe it. Much of what physicians know about drugs comes directly from pharmaceutical companies promoting a product. Because pharmaceutical companies don’t manufacture natural hormones, most physicians do not learn about them unless they do personal research, and education.” “Where does one fill prescriptions for natural hormones? There is a special type of pharmacy known as a compounding pharmacy. These are regular licensed pharmacies that are capable of providing you with any drug from pharmaceutical companies. But compounding pharmacies are able to do more. They are able to use the pure pharmaceutical grade hormone and compound it into the specific dose and form ordered by the physician. They can produce pills, capsules, liquids, and creams. This type of program is highly customized and personalized.” “To summarize, a bioidentical hormone has a chemical structure that is identical to the hormone naturally produced by the body. We refer to them as natural because they are natural to the human body. Natural hormones cannot be patented by drug companies. Synthetic hormones have a structure similar to but not exactly the same as a hormone produced by your body. These chemical differences mean that the synthetic hormone acts differently and produces substantially different effects. Natural (bioidentical) and synthetic hormones should not be considered the same or used interchangeably. They are entirely different. A multitude of studies have demonstrated many harmful effects of synthetic hormones whereas the medical literature supports no harmful effects of natural hormones, only beneficial effects.” “More people are beginning to realize that they no longer have to accept the fact that their health, appearance and function must deteriorate. They no longer want to accept growing frail and feeble...Science is creating a new paradigm of preventive medicine by allowing our bodies to remain stronger, healthier, and more vigorous... "Hormone replacement therapy, however, is not a panacea. It will not reverse aging. It will not keep us permanently at one age. We will still continue to age and lose cells secondary to a process that is regulated genetically. With hormones we may be able to slow the precipitous decline that occurs after midlife; no sudden falling off in our physical and mental health. We hope to stay resilient. We aim for a gradual transition that will be less noticeable that it would be without hormone replenishment. The purpose is to simply replenish the hormones that already occur naturally in our body and boost them back up to the appropriate medically sound levels necessary to maintain youthful health and vigor. Which hormones to replenish, how much to replenish and how to adjust the hormones so that they have a synergistic effect is the art and science of the specialty of natural hormone replacement medicine, which is a key aspect to preventive medicine.” Much appreciation to Neal Rouzier, MD, with whom I studied extensively to learn this very interesting area of medicine. Many people ask me on a daily basis about Vitamin D and what is its importance.
Despite its name, vitamin D is not a vitamin, but a steroid hormone made in the skin, (from cholesterol). The normal range is pretty wide, from 30 to 100, and it’s better to work up to the higher levels than maintain at the lower levels. It’s usually pretty easy to get to “normal” levels by taking up to 50,000 units of vitamin D3 a week for up to 8 weeks and then maintain at 1000 to 5,000 units daily. 57% of patients in once study were judged to be vitamin D deficient, including 37% who consumed more than the recommended amount of vitamin D (at least 800 IU/ day). Although vitamin D can be obtained through the diet, most foods contain very small amounts, so humans are dependent on skin production to maintain normal levels ( or, with the addition of daily supplements.) Vitamin D deficiency is important to understand in age-related morbidities. Meta-analysis of double-blind randomized trials showed that vitamin D reduced the risk of falling by 22%. Low Vitamin D levels play a role in bladder incontinence, because there is poorer coordination of the muscles used to control urination. Low levels also play a role in age-related macular degeneration as well asl cognitive decline. The lower the vitamin D, the greater the incidence of sarcopenia, or bone loss. Men and women with baseline levels less than 25 no LVH/L were more than twice as likely to develop sarcopenia. Increasing the levels of serum vitamin D regardless of age, may reduce the risk of breast cancer. Vitamin D level of 35 ng/ml has associated with a 20% reduction in the risk of breast cancer. In another study, average levels of 52 ng/ml had 50% lower risk of breast cancer than those with serum vitamin D of less than 13 ng/ml. Vitamin D intake of 2,000IU/day has been associated with vitamin D levels of 32 ng/ml. The higher level noted above corresponded to an intake of 4,000 IU of vitamin D per day. Vitamin D may provide greater health benefits than previously thought, benefits that include not only improved bone health, but other effects as well. Increased vitamin D levels may decrease the risk of cancer, especially that related to colorectal adenomas. Elderly adults may even benefit from higher doses such as 2000 IU to 5000 IU daily. Vitamin D levels of 82 nmol/L and higher were also associated with a 50% lower risk of developing colorectal cancer. Some researchers are advocating even higher doses, up to 10,000 IU per day. Lower levels of Vitamin D are associated with a higher risk of heart attack in a graded manner. High levels of vitamin D among middle-age, and elderly populations are associated with a substantial decrease in cardiovascular disease, type 2 diabetes and metabolic syndrome. Vitamin D has been traditionally related to bone metabolism, although several studies in the last decade have suggested its role in muscle strength and falls, cardiovascular and neurological disease, malignancies, autoimmune diseases and infections. Vitamin D appears to be a hormone with several actions and is fundamental for many biological systems including bone, skeletal muscle, brain and heart. It helps to maintain physical strength in the elderly and is protective against falls. Additionally, a study demonstrated that women with moderate to severe depression had substantial improvement in their symptoms of depression after they received treatment for Vitamin D deficiency. Both the presence and severity of depression were associated with decreased serum levels of vitamin D and increased levels of parathyroid hormone in older patients. In a paper called Vitamin D for cancer prevention: Global Perspective, higher levels of vitamin D were associated with substantially lower incidence rates of colon, breast, ovarian, renal, pancreatic, aggressive prostate and other cancers. It was projected that raising the minimum year- around levels to 40 to 60 ng/ml would prevent approximately 58,000 new cases of breast cancer and 49,000 new cases of colorectal cancer each year, and three fourths of deaths from these diseases in the United States and Canada. I hope that this little essay helps you understand and appreciate further the role of vitamin D. This is a lecture that I prepared and I thought it would be enjoyable to read in this “slide show” format. It gives really good information regarding testosterone and how it interacts with the prostate. However, this is not fully accepted in the Urology community. I guess I’ve always been somewhat iconoclastic, but I sure have enjoyed the dozens and dozens of hours I’ve spent in studying these and other topics in great depth to learn what many docs don’t know. Click the link below to download the presentation. I hope you enjoy reading through this! Brian Chesnie, M.D.
I enjoy writing educational essays in this website to hopefully provide interesting reading material to my patients. I have previously written essays that include an overview of issues pertaining to prevention and how to achieve well-being. Included was an introductory essay of how your body’s natural hormones play important roles throughout life in maintaining the strength and well- being of your body. Over the past year I have taken a number of educational seminars and study in the area of optimizing your own body’s hormones to help improve health and well-being. I’d like you all to know that I have recently written the exam and passed with flying colors and am now certified in this interesting area. Following is an essay overviewing the benefits as well as the myths pertaining to testosterone therapy. This essay is derived from numerous peer review papers in the medical literature which convey significant benefit of testosterone therapy, and this essay will also touch upon some of the negative papers that achieved much media attention and conveyed significant misperceptions about this subject. I recently gave this talk at Cardiovascular Conference to the Department of Cardiology at Hoag Memorial Hospital. WHAT IS TESTOSTERONE? Testosterone is a hormone secreted by the ovaries, the adrenal glands, and the testes. The “Normal Range” is portrayed at about 250 to 900 pg/ml. This is an arbitrary setting based on up to 20 men in the 50 to 80 year old range. The ranges would be considerably higher in the healthy 20 to 30 year old group: consider about 500 to 2000! Depletion of testosterone with aging (testosterone deficiency) includes symptoms of diminished libido, sense of vitality, erectile dysfunction, reduced muscle mass and bone density, mood change, depression, and anemia. CONFUSION AND MISPERCEPTIONS ABOUT TESTOSTERONE: There are 2 papers in the medical literature written in 2013, and 2014 that received enormous media attention. These have determined to be very flawed papers, written with very faulty statistical design and flawed methods and conclusions. They both initially suggested that there was an increase in cardiac events such as heart attacks and strokes, but further analysis demonstrated incorrect interpretation of the numbers and incorrect conclusions. In fact 29 societies and 50 international experts have called for the retraction of these papers. One paper has had to make 3 corrections with apologies, and when re-done it actually showed that testosterone lowered the percentage of adverse cardiovascular events. The second paper had no control group, and in fact, it was based on merely handing out a testosterone prescription and did not assess whether the men were actually taking it! One of the big confusions is that doctors think that testosterone increases the risk of clotting and what it does to the blood. This is simply not true. The confusion is many doctors think that testosterone can cause a blood disorder called Polycythemia, which can increase the risk of clotting. This is because Polycythemia causes an increase in hemoglobin and hematocrit, (red blood cells) as well as an increase in white blood cell count and increase in platelets. It is the increase in platelets that causes the increase risk of clotting. Testosterone at high levels may increase the level of hemoglobin and hematocrit (red blood cells which carry oxygen to your cells)! This is something called “erythrocytosis”. Testosterone does not increase the level of white cells nor platelets and therefore does not increase the risk of clotting. In fact, over 200,000,000 people on the Planet Earth may have “erythrocytosis” because they live at over 7,000 feet above sea level and they don’t have an increased risk of clotting. In fact, the US Olympic athletes often train in Colorado at elevation in order to boost their hemoglobin and hematocrit! It is not uncommon for the Sherpas who carry heavy loads in the Himalayas to have very elevated hemoglobin and hematocrit. They do not have an increased risk of blood clots. Since those two studies, more than a dozen clinical trials and observational studies have provided additional information, with none demonstrating increased cardiovascular risk. On the contrary, several of these studies have suggested that testosterone therapy may be cardioprotective. Following are some examples: PUBLICATIONS ON THE BENEFITS OF TESTOSTERONE: A recent paper published in the Journal of Cardiovascular Pharmacology and Therapeutics by Traisch in 2017 compared a group of higher cardiovascular risk men treated with testosterone versus placebo: 360 men treated versus 296 on placebo; a 10 year follow-up. The treated group had a significant lower incidence of death, heart attacks and stroke than the placebo group. Also noted was a reduction in waist circumference, and body weight, improvement in lipid profile and reduction of blood glucose. In fact, the placebo group had 26 nonfatal heart attacks and 30 nonfatal strokes and the testosterone treated group had none. There were 21 deaths in the placebo group: 19 cardiovascular events including 5 heart attacks, 4 strokes, 7 heart failures, 2 thromboembolism, 1 Pulmonary embolism. There were 2 deaths in the testosterone treated group: 1 person died after a surgical procedure, and 1 person died in a car accident. A series of papers called the Testosterone Trials showed at 2 year of follow up, 8 heart attacks in the placebo group, and 1 heart attack in the testosterone treated group. There were improvements in cholesterol levels, blood sugar levels, blood pressure, heart rate, weight, waist circumference...and these were added benefits in addition to the presence of statins. Another paper showed an 8 year weight loss of 17-24% with testosterone therapy comparing favorably to the 10 year weight loss of 14%-25% seen with bariatric surgery. The Testosterone Trials were published in the New England Journal of Medicine in 2016. They were a set of 7 double blind placebo-controlled trials at 12 sites. The studies were built around inclusion criteria of sexual function, physical function and vitality in 790 men over the age of 65. These men had issues of obesity, high blood pressure, diabetes, some were smokers, and a number even had previous heart attacks: they were considered to be a high risk group. Androgel, a fairly weak commercial product was used and more or less doubled the testosterone levels from around 230 to 250 to about 500 ng/dL (nothing stellar!). The testosterone group versus placebo group showed improved sexual desire, increase in sexual activity, and improved erectile function. There was improvement in walking distance and duration. There was an improvement in energy, mood, reduction in depression; improved muscle strength and bone density. Over 2 years, cardiovascular events including heart attack, stroke, and death due to cardiovascular cause were 9 in the testosterone treated group and 16 in the placebo group. (3 deaths in the testosterone group, 7 in the placebo group.) SO WHAT DO WE KNOW ABOUT THE BENEFITS OF TESTOSTERONE?
In fact, testosterone is banned in the Olympics and professional sports due to the fact that it improves strength, it increases muscle mass, it increases endurance, and it may therefore improve athletic performance. TESTOSTERONE IN WOMEN: Testosterone for women has the same beneficial effects as it has for men. It improves well-being, energy, strength and endurance. It improves body composition, decreases visceral and subcutaneous fat, and improves bone density. It maintains muscle mass which helps maintain better metabolism. This is beneficial for prevention of diabetes and heart disease. It may improve sexual function and increases orgasmic ability. It increases collagen in skin with increased skin thickness, improved texture, decrease in wrinkles and decrease in fat deposition and cellulite. It is indicated for any woman who wants to improve health, wellness, strength, confidence aesthetics, metabolism, fat loss, sexual function, and breast cancer protection. It is contraindicated in pregnancy, planned pregnancy, breast feeding, and physician resistance! HOW TESTOSTERONE IS SUPPLIED:
My preference is with the compounded creams because they are well absorbed, maintain higher and consistent levels without a “peak and trough” effect. CONCLUSION: When the full literature is reviewed and studied, the overwhelming trend is very much in favor that testosterone at a minimum does not harm in terms of cardiovascular risk, and indeed there is an abundance of evidence that it offers significant benefit to cardiovascular risk factors, and outcomes. The 2 papers that suggested a negative interaction have been highly criticized and found to be flawed in their presentation, analysis, and conclusions. There are several dozen papers in the literature that show significant benefit. Additionally, are the added benefits of well-being, energy, libido, sexual function, muscle mass, diminished fat, skin tone, improved bone density. This is a hormone that is intrinsic to both males and females. It offers benefits to both. However, only males have prostates and this is another area where misinformation and confusion abound in the relationship of testosterone to prostate cancer. I will next go into a full discussion of this topic-something the medical community at large does not know much about- in my next blog, which will follow shortly. 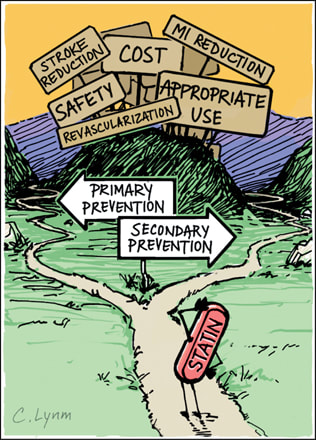 On a daily basis I encounter patients who refuse to take statin medications. The Internet provides so much information and misinformation that mythologies abound and it is very hard to sift through what is meaningful and what is not. This blog contains a lot of information: it is everything you wish to know or don't want to know about the importance of statin therapy. The class of drugs known as statins was discovered by Dr. Akira Endo at Sankyo in Japan in the early 1970’s. It inhibits the enzyme 3-hydroxy-methylglutaryl-coenzyme A (HMG-CoA) reductase. Merck&Co. launched the first statin made available to the public, lovastatin (Mevacor) in 1987. Lovastatin and the other statins that followed have resulted in a substantial reduction in virtually all clinical manifestations of atherosclerotic vascular disease, including coronary events, strokes, and revascularization procedures, and have prolonged the lives of millions of people. Of the 6 most commonly used statins, 3 are derived from fungi (lovastatin, simvastatin, and pravastatin, and 3 are synthetic (fluvastatin, atorvastatin, and rosuvastatin). As mentioned, statins block or “inhibit” HMG-CoA in the liver and this blocks a protein called mevalonate, which then suppresses the manufacture of cholesterol; the stronger the statin, the more mevalonate that is inhibited. Additionally, the more this occurs (with the stronger statins) more LDL receptors are manufactured in the liver cell to go to the cell surface to remove circulating LDL into the hepatocyte (liver cell) and degrade the LDL into bile acid. Statins have a significant lipid lowering effect and have significantly lessened the event rates of coronary artery and other arterial diseases. It must be noted that though 1/3 to 1/2 of those who take statins have benefit in outcome, 1/2 to 2/3’s do not. Though the reduction of cholesterol and LDL levels are proposed as the primary principle for arterial protection, it is not the sole mechanism for benefit. There are several actions that are independent of cholesterol lowering: 1)Statins improve inflammation in the artery wall and can improve features associated with plaque stability. 2)Blood C-reactive protein (CRP), a marker of inflammation is reduced by statins independently of the amount of cholesterol lowering. 3)Statins improve endothelial function rapidly, before any appreciable reduction in serum cholesterol can be detected. (The endothelium is the lining into the artery wall). 4)Statins reverse endothelial dysfunction in young smokers with normal LDL levels. 5)Regression of coronary atherosclerosis, and improvement in clinical outcomes with intensive statin therapy are related equally to reduction of CRP and other inflammatory markers as well as LDL cholesterol regulation. If statins offer benefits that are independent of cholesterol lowering, how does this occur? There are a group of complicated protein interactions (the rho proteins), that influence cellular membrane metabolism. This process triggers much of the atherosclerotic process: reduction of nitric oxide, acceleration of vascular inflammation, increased levels of inflammatory proteins, increased vascular smooth muscle proliferation, increased levels of thrombotic (clotting) factors. (Plus many more very complex cellular and biochemical interactions). Statins interact with and reduce these Rho proteins . This produces a decrease or even a complete reversal of most of the atherosclerotic cellular processes listed previously. This is a very important arena of science and clinical research. Lipid Effects: The evidence that lowering LDL cholesterol reduces cardiovascular events is very strong!: Statins are the preferred first line treatment of choice for coronary disease risk reduction within the context of pharmacological therapy. The concept of “lower is better” is supported by a lot of data. The statins differ in their LDL lowering capability. This was demonstrated in the STELLAR trial (Statin Therapies for Elevated Lipid Levels Compared Across Doses to Rosuvastatin). This was a randomized, parallel -group, open label, comparator-controlled trial of 2431 hypercholesterolemia adults to compare lipid changes after 6 weeks for all of the statins and doses tested: Rosuvastatin lowered LDL cholesterol across its 10 to 40 mg dose range by 46% to 55%, compared with 37% to 51% for atorvastatin 10 to 80 mg dose range, 28% to 46% for simvastatin 10 to 80 mg dose range and 20% to 30% for the pravastatin 10 to 40 mg dose range. This LDL lowering effect is reflected in their ability to attain the earlier National Cholesterol Education Program Adult Treatment Panel 111 (NCEP ATP111) LDL goals. Again, from STELLAR, the percentage of coronary heart disease patients who achieved treatment goal of less than 100 mg/dl with Rosuvastatin 10 mg, Atorvastatin 20 mg, Simvastatin 40 mg and Pravastatin 40 mg were 55%, 43%, 31% and 11% respectively. Another example of statin effectiveness to achieve LDL lowering to less than 100 mg/dl was studied with Rosuvastatin in a group of patients with very high LDL levels from 190 to 240 mg/dl (this group has heterozygous familial hypercholesterolemia). Rosuvastatin 10 mg lowered LDL to less than 100 in 37% of patients, and 20 mg lowered LDL to less than 100 in 66%. Statins also lower triglycerides, generally in the range of 15 to 30%, also in relation to the strength of the statin in lowering LDL. Generally, the greater the baseline triglyceride , the greater the lowering. Patients who have triglycerides of greater than 200 tend to have a more aggressive lipid atherosclerotic pattern. This goes along with metabolic syndrome which is a pre-diabetes picture: High levels of triglycerides, low levels of HDL, increased VLDL particles, and LDL particles that are smaller, more dense, and greater in number which are more aggressive in the atherosclerotic profile. Statins have been shown to be effective in improving all of these parameters. By their very mechanism of action, statins remove VLDL and LDL particles from the circulation. There is not only reduction in concentration of particle number of LDL and VLDL but also a preferential removal of smaller dense LDL particles. In one study, atorvastatin removed 44% of small dense LDL particles and 10% of larger particles and 31% of all LDL particles. By contrast, niacin, a drug used for patients with this more aggressive atherosclerotic profile, shifted small LDL particles to larger ones and reduced particle number by 14%. Niacin does have a beneficial effect on increasing HDL levels by 10% to 15%. Rosuvastatin may raise HDL to 8% to 10%. Impact on Morbidity and Mortality Statins have been evaluated in more than 100,000 individuals participating in randomized, controlled clinical event end point trials: over 18 large population studies, both primary risk prevention studies (no coronary or arterial event has occurred yet) and also secondary risk prevention studies ( the event has occurred, and we’re trying to prevent the next one). The conclusion for all of these studies is that all outcomes of atherosclerotic vascular disease is reduced with statin therapy including coronary artery disease death, non-fatal MI, coronary revascularization, acute coronary syndrome, unstable angina, stroke, peripheral vascular disease, cardiac arrest, and heart failure. Reductions in total mortality have been specifically documented in 4S, LIPID (Long Term Intervention with Pravastatin the Ischemic Heart Disease), and HPS (Heart Protection Study). Several of the Primary Prevention studies include: 1.the ALLHAT Study with 10,335 adults double blinded to placebo or Pravastatin 40 mg/day. There was an average of LDL lowering of 17% and a lowering of coronary or stroke events by 9% over 4.8 years. 2.the ALERT study with 2100 adults on placebo or Fluvastatin 40 mg/day showed an average lowering of LDL of 32% and a lowering of coronary events of 35%. The average reduction of cardiac death, nonfatal MI and revascularization was 17%. Followup was 5.1 years. 3.the ASCOT trial included 14,350 adults treated with placebo or Atorvastatin 10 mg. the LDL average lowering was 35% and reduction in CHD events was 31% with followup of 3.3 years. 4.SPARCL with 4731 adults treated with placebo or Atorvastatin 80 mg had LDL lowering of 45% and a reduction of coronary events of 35% over 4.9 years. 5.WOSCOPS trial with 6595 men, treated with placebo or Pravastatin 40 mg daily. LDL lowering was averaged at 26% and coronary events lowered by 31% over 4.9 years. 6.AFCAPS/TEXCAPS study had 66065 adults treated with placebo or Lovastatin 20 to 40 mg day . LDL lowering averaged 25%, and coronary event lowering averaged 40% over 5.2 years. Secondary Prevention studies are studies where a coronary vascular event has already occurred. Some of these studies are: 1.4S: 4444 adults treated with placebo or Simvastatin 40 mg daily. LDL lowering was 35%, coronary event reduction was 34% over 5.4 years. 2.LIPID: 9014 adults treated with placebo or Pravastatin 40 mg. LDL lowering was 25% and coronary event reduction was 24% over 6.1 years. 3.CARE: 4159 adults treated with placebo or Pravastatin 40 mg. LDL lowering was 32% and coronary event reduction was 24% over 5 years. 4.HPS: 20,536 adults treated with placebo or Simvastatin 40 mg. LDL lowering was 32% and coronary event reduction was 27% over 4.9 years. 5.TNT: 10,000 adults treated with placebo, or Atorvastatin 10 mg vs. Atorvastatin 80 mg. Further drop in LDL lowering of 24% and a further reduction in coronary events of 22% over 4.9 years. It is important to comment that all of the above dramatic percentage drops in LDL lowering and disease event rates are not percentages based on the total number of patients. These reductions are called relative risk reductions and an example would be the following: Of 10,000 patients, 200 patients taking placebo had a cardiovascular event, and 100 patients taking statin had a cardiovascular event. That would represent a 50% reduction based on RELATIVE RISK criteria which in clinical double blind randomized studies MUST achieve statistical significance by at least 0.05%. This is based on the numbers in the study, the percentage of people responding, and the length of time of the study. It would be a mistake to think that in a 10,000 person study, 7000 had coronary events on placebo and 3000 had events on statin. That is something that never occurs in these types of studies. The statins are effective at reducing cardiovascular event rates in patients with existing vascular disease (secondary prevention) as well as those with only risk factors (primary prevention). Statins are equally effective in reducing risk and events in men and in women, irrespective of age. Statins are effective in reducing events in diabetic patients. Patients with diabetes or metabolic syndrome often have atherogenic dyslipidemia with only modestly increased LDL. In spite of this, statins are excellent treatments of choice in these patients because they effectively reduce small dense LDL particles, cholesterol-enriched remnant particles and overall particle number as discussed above. The Collaborative Atorvastatin Diabetes Study (CARDS) specifically studied type 2 diabetic patients and reported a 37% relative event reduction which was so robust that the trial was stopped prematurely. In 2012, there was a departure from the original NCEP ATP111 recommendation of driving LDL to less than 100 in intermediate risk patients and to less than 70 in higher risk patients. Though the National Lipid Association and several European cardiovascular societies have maintained this recommendation, the American College of Cardiology presented a new recommendation of achieving a 30% lowering of LDL from baseline in intermediate risk patients and a greater than 50% reduction in the higher risk groups. Though there is considerable debate amongst the various professional groups, the primary caveat is the importance of LDL lowering through diet and exercise programs and then utilizing pharmacologic tools with statins as the primary recommendation. OTHER ISSUES: Alzheimer’s Disease. Alzheimer’s Disease is a neurodegenerative disorder that leads to cognitive decline and neuropsychiatric symptoms and diffuse structural abnormalities in the brain. It is characterized by the deposition of amyloid plaques and neural fiber tangles that may be related to cholesterol synthesis. Evidence that links cholesterol and Alzheimer’s Disease has come from observational studies. It has been observed that an elevated cholesterol level in mid-life increases the risk of Alzheimer’s Disease to 2 to 3 fold in later life. Conversely it has been observed that people who take statins and other lipid-lowering agents have a 60% to 75% reduction in the future risk of Alzheimer’s Disease. Liver. Elevation of liver enzyme blood tests to greater than 3 times normal with statin therapy are rare. In one meta analysis of 74,102 patients the incidence of this was 1.4% in statin treated patients and 1.1% in placebo control patients. It appears to be more related with the intensity of the statin dose rather than the degree of LDL lowering. It also tends to be transient. In an analysis of 180,000 people it was reported that 300 in 90,000 treated with a statin had elevations of 3 times normal. Of the 300, only 110 had consecutive elevations with another repeated blood test. The incidence of actual liver failure is extremely rare. In the FDA Adverse Event Reporting System (AERS), it was calculated that there was 1 case in 1.4 million patient-treatment-years. In fact the incidence of 1 case per million is the same in patients taking a statin as well as with people NOT taking a statin. In the context of a 3 fold increase in liver enzyme blood tests it is considered prudent to interrupt statin therapy for a brief period of time and reassess lab values and then resume therapy. It is recommended that the clinician evaluate clinical symptoms and signs of liver dysfunction ( malaise, fatigue, loss of appetite, weight loss, jaundice). It the blood tests normalize or if the blood tests are only mildly elevated, then the statin therapy may be resumed, or in the latter case, not interrupted. The position of the National Lipid Association is that interruption of statins with mild elevation of liver blood tests (<3 times normal) to avoid a very remote risk of liver failure, the patient will be exposed to a disproportionally higher risk for cardiovascular events. Patients with nonalcoholic fatty liver disease have a significantly increased cardiovascular risk and are candidates for statin therapy. Statins are actually safe in these patients. Statins do not further elevate baseline liver enzyme abnormalities, and in fact may actually improve liver function. Muscle. The 2 more serious muscle problems are myopathy (muscle discomfort, pain, weakness, with an elevation of creatine kinase (CK) to greater than 10 times upper limit of normal, and rhabdomyolysis ( the above with associated kidney failure and higher risk of death). These serious muscle-related adverse effects are rare. In an analysis of 21 randomized clinical trials with 180,000 person-years of followup on statin therapy or placebo, myopathy occurred in 5 patients per 100,000 person-years, and rhabdomyolysis in 1.6 patients per 100,000 person-years. The AERS database reported a rate of 0.3 to 2.2 cases of myopathy and 0.3 to 13.5 cases of rhabdomyolysis per 1 million statin prescriptions. Muscle toxicity with statins is a class effect but there appears to be a difference between weaker and stronger statins. Pravastatin was not associated with a case of rhabdomyolysis in 19,768 people studied for 5 years. Simvastatin produced rhabdomyolysis in 0.1% of 2265 patients on 80 mg in the A to Z trial. The more common adverse effect of statins is myalgia, which is muscle soreness, pain, or weakness. This is not associated with the above serious complications of myopathy or rhadbomyolisis. The incidence of myalgia varies between 5% to 15% in the literature. There tends to be some misinformation as to the accuracy because there is often confusion about what constitutes statin related myalgia, versus a localized sore muscle or joint, related to activity or arthritis. Reports of myalgia with statins in clinical trials are the same as, or only slightly more than, those reported in patients receiving placebo. However, this complaint is the most common reason for patients to discontinue therapy. A specific gene has been discovered that affects liver uptake of statins. This gene (rs4363657) occurs in about 15% of the population. With this gene, statins would not be taken up as freely into liver cells thus elevating statin blood levels. Also higher statin doses, and drug interactions may also increase the statin blood level and thereby increase the risk of muscle achiness. Some investigators have related the cause of myalgia and myotoxicity to a drop in ubiquinone levels. This is also known as coenzyme Q10 (CoQ10). Ubiquinone plays a role in cellular energy and cell membrane activity. It is carried in LDL particles and thus, with lowering of LDL levels there is also a lowering of CoQ10 levels. There is some conflicting data as to the measurement of CoQ10 levels in muscle cells, and the lowering effect related to dosage of statin. There have been conflicting results on the benefits of giving CoQ10 to patients to prevent or to treat muscle-related symptoms. In one study that used high doses of lovastatin, supplementation with CoQ10 240 mg daily did not reduce the frequency of myalgia compared to those not receiving it. In another study, statin-taking patients who had myalgia had their pain assessed on a 10 point grid. Those given 100 mg daily CoQ10 had reduction of 5 to 3 with the addition of this: Somewhat equivocal! However, there are no known risks associated with taking CoQ10. Giving patients CoQ10 may be tried in patients who develop myalgia and cannot otherwise tolerate statin therapy. The clinician should also be aware of anything that can elevate statin blood level. This would include higher dosage, older age, frailty, female gender, renal insufficiency, hepatic dysfunction, hypothyroidism, and use of other pharmaceutical agents that have interaction with statins. I’ve addressed before the complexity of the disease called “Atheroscelerosis”. I’ve discussed how it can smolder and develop over decades and then how it can suddenly erupt: with a ruptured plaque causing an acute coronary event. In preventive cardiology, we are committed to impacting this mysterious and complicated process. There are 3 objectives: first is to try to slow down the atherosclerotic process, second is to stop it, and third is to reverse it. When people are unable or unwilling to engage in the science of pharmacology, they are removing very important ammunition to engage this unrelenting disease. Obviously there are many facets that are called into play: appropriate nutrition, exercise, weight management, avoidance of diabetes, hypertension and smoking. Most people know what to do as regards these behavioral issues, how many are successful in conquering these issues? I’ve learned that optimization of your body’s hormones plays an exceptional role as well, but when overt bias exists that is oppositional to the gift that the science of pharmacology has given us, why would you put yourself in a position whereby you are not giving yourself the best opportunities to counter this difficult and unpredictable disease? The bibliography to the above essay is obviously very extensive and is not listed here. However, much of the essay was synthesized from the chapter on Statins, written by James McKenney, Peter Ganz, Barbara Wiggins, and Joseph Saseen in the textbook of Clinical Lipidology, edited by Christie M. Ballantyne. I recently attended a symposium that was taught by Neil Rouzier, MD, an internationally renowned authority in the field of Hormone Optimization. It was called “Mastering the Protocols For Optimization of Hormone Replacement Therapy”.
I spent many hours studying the literature and science regarding the importance of the key hormones circulating in our bodies and how they relate to normal physiology and the maintenance of good health. Most of our hormonal levels decline with age: Dehydroepiandrosterone (DHEA), melatonin, triiodothyronine (T3), estradiol, progesterone, testosterone, and growth hormone. The highest levels occur when we are in our twenties, and as we age, the normal ranges diminish and are by no means the optimal levels that cultivate good health and well-being. With aging comes a diminished capacity for cellular protein synthesis and a decline in immune function, an increase in fat mass, a loss of muscle mass and strength, and a decrease in bone mineral density. Physical frailty includes falls, fractures, impairment in activities of daily living and loss of independence. Osteoporosis, sedentary life style and chronic debilitating diseases are all important factors in the process of frailty. The link between obesity and diseases of aging has been well confirmed in numerous studies. These experiments provide powerful evidence that visceral fat tissue has direct effect on age associated insulin resistance. The increase in visceral fat tissue in older people is associated with decrease in serum levels of estrogen, DHEA, testosterone and growth hormone. Augmenting the lower levels of these and other hormones that decrease with age may better control visceral fat deposition, thereby leading to decreased insulin resistance and to decreased risk of diabetes and atherosclerosis. Our orientation in medicine has always been to diagnose and treat a disease process. Many of these disease processes: cardiovascular disease, stroke, cancer, and Alzheimer’s disease have all been blamed on the aging process. Conventional medicine has never treated aging as a “disease process” nor has it tried to alter the outcome of the aging process. For over 10 years my practice has evolved from diagnosis and management of serious cardiovascular problems to also include a very major commitment to the prevention of cardiovascular disease expression and to try and alter and improve outcomes. All of my patients know this because this “Prevention Perspective” is part of my daily conversation and this was why I made the decision to become Board Certified in Clinical Lipidology 10 years ago. Though I have learned and developed great skills in working on the heart and cardiovascular system, and on the electrical system of the heart, most of my patients know that I have always tried to be more of a complete physician than just working on just the specific organ system alone. If I have practiced as a cardiovascular disease prevention doctor, then I have concluded that numerous aspects of trying to improve health and well-being are required: nutrition, exertion activity, developing psychological and relationship well-being, challenge in career, and the judicious and careful use of medications. The optimization of your body’s hormones is also an intriguing concept that can reap beneficial dividends. All the hormones mentioned earlier are responsible for the regulation of the body’s temperature, growth, muscle and bone development and maintenance, sexual desire, well-being, healing, immune function and aging. The neuro-endocrine system allows for communication with every cell in the body. Hormone deficiencies affect every cell in the body and participate in the degenerative changes of aging. Optimization of these natural hormones (not synthetic) may demonstrate improvement in so many things: Growth Hormone (hGH) is produced by the pituitary gland and is processed in the liver and converted into a protein called insulin-like growth factor-one or IGF-1. It contributes to ongoing tissue repair, healing, cell rejuvenation, bone strength, brain function, enzyme production, and the integrity of hair, nails, and skin. All major hGH studies have documented improved body composition and function. There is a consistent improvement in muscle/fat ratio. There is a 10 to 20% decrease in fat and a 10% increase in muscle. There is also an increased breakdown of fat with concomitant decrease in cholesterol and triglycerides. There is an increase in exercise capacity, bone density, muscle mass and strength. DHEA is a hormone secreted by the adrenal glands. It cultivates a “protein building state”. It reduces cardiovascular risk by increasing the breakdown of fat. It may help reverse the deleterious effects of stress on the immune system, and may help restore sexual vitality, and improve mood. Melatonin is secreted by the pineal gland. It activates at night, in the dark, and affects patterns of sleep. We know that the cells of the body rejuvenate and repair during the deeper stages of sleep. Melatonin helps increase the deeper stages of sleep and this helps enhance immune function. It also has powerful antioxidant effects. Thyroid hormone: the thyroid hormone that binds to cell receptors and then enters the cell is not thyroxine (T4) but triiodothyronine (T3). Thyroxine upgrades to triiodothyronine on a 4:1 ratio. It contributes to energy levels and temperature regulation and body warmth. Higher normal levels increase fat breakdown, resulting in weight reduction and lowering of cholesterol. It protects against cardiovascular disease and improves cerebral metabolism. It helps to prevent cognitive impairment. Testosterone is a hormone secreted by the adrenal glands, testes and ovaries. It contributes to muscle mass, strength and endurance, decreased fat, increased exercise tolerance, enhancement of well-being and psychological status. It protects against cardiovascular disease, hypertension, body fat and arthritis. It leads to improved lean muscle mass, increased bone density, decrease in cholesterol, improved skin tone, improved healing capacity and increased libido and sexual performance. It is also present and extremely important in the female as well as the male. Estrogen is secreted by the ovaries. Estrogen (and we specifically mean estradiol), protects against heart disease, stroke, osteoporosis, Alzheimers Disease and memory disorders. It protects against vaginal atrophy, urinary incontinence, and prevents symptoms of menopause, including hot flashes and temperature disregulation. Estrogen deficiency results in urogenital atrophy, incontinence, sagging skin in the breasts, increased skin wrinkles of the face, increased fatigue, depression, decreased libido. Most importantly, the estrogen prescribed must be a natural estrogen, (estradiol) not a synthetic estrogen (Premarin). The synthetic estrogens have been shown to be harmful. Progesterone is secreted by the ovaries and reduces symptoms of menopause. It protects against uterine cancer and breast cancer, osteoporosis, and ovarian cysts. The problem is that most U.S. physicians prescribe synthetic progestins, which cause numerous side effects such as bloating, headaches, fatigue and weight gain. Natural progesterone must be prescribed in place of synthetic progestins (a different molecule) to avoid these side effect issues. Hormones are not drugs. They are natural substances that have existed in our bodies even before birth. The depletion of them contribute to the deleterious aspects associated with aging, and the maintenance of them to optimal levels may help the countenance of well-being, energy, improved health, improved cognition, better stamina, better libido, and maintenance of body integrity as we age. It is imperative that these replacement hormones be natural, micronized, and produced at the highest quality pharmacies that maintain certification with all appropriate licensure and certification for pharmaceutical grade products. If this is the case, then you are guaranteed that the molecule of the hormone and the delivery of the hormone is consistent, standardized, and reproducible. As a cardiologist who has focused on not only the critical care of disease management but also the committed care of disease prevention, and then extrapolating that into improved health and well-being, I felt it was imperative that I present this discussion to those who may wish to inquire into the possibility of improved quality of life.
In Part 1, I brought attention to many of the universal human conflicts that we all struggle with, how they may disrupt and create turmoil in our inner world, and the consequences that these have directly on our health. In Part 2, I discussed both particular as well as general guides on the issues of nutrition, weight reduction, and exercise, and what needs to be done to truly impact your physical health in general and your cardiovascular health in particular. Part 3 concludes that there is more to it than that. Living long and living well requires purposeful tasks, some accommodation to self-understanding, striving, and sense of purpose, and equally important, how do you get along with others? What is your sense of "relatedness" to others? But, you also have to be lucky! Here's a little story: I took care of an old fellow for over 22 years. When we met, he had just survived a cardiac arrest while jogging, and he had had a heart attack. He had a coronary bypass operation, also surgery for an implantable cardioverter /defibrillator, and eventually 2 further stents. For over 18 years, he lived well, stayed thin, ate responsibly, continued to exercise, took the "right medications" and enjoyed life. One day not too long ago he came to see me. He was now 88. He looked ill. He had been diagnosed with non-Hodgkins Lymphoma, and he had already begun a chemotherapy program that was making him very ill. He was struggling and we talked about a number of things, and he asked me what my thoughts were. I said, "Jerry, this is the curse of having had a good cardiologist!" He laughed and we both realized that we are all going to end up with something that makes us mortal! Having done this for over 35 years now, I have come to appreciate that this life we have is the only one that we have got, and it is so important to try and (as well as to) live it the best we can. What might be some of the other factors that can help people live life well? Do you think there is an importance to education? There is a lot of data on this. People with greater than 16 years of education have longer mean life spans than people with less than 12 years. For example, in women, Caucasians by 10.4 years, African Americans by 6.5 years , Hispanics by 2.9 years. In men, Caucasians by 12.9 years, African Americans by 9.7 years, Hispanics by 5.5 years. "Education exerts its direct beneficial effect on health through adoption of healthier lifestyles, better ability to cope with stress, more effective management of chronic diseases...the indirect effects of education through access to more privileged social position, better paying jobs, higher income..."(Moeller, P. US News and World Report, 8/16/12) What are the effects of marriage on health? Here is a synthesis of recent research evidence published by the US Dept. of Health and Human Services (06/2007): * Marriage has become an increasingly important topic in academic and policy research. A burgeoning literature suggests that marriage may have a wide range of benefits, including improvements in individuals' economic well- being, mental and physical health, and the well-being of their children... * Health behaviors: Reviewing behaviors that have well-documented connections with physical health outcomes: alcohol and drug use, smoking, weight and exercise. * Health Care access, use and costs: Examining the link between marriage and 3 main health care outcomes: 1) health insurance status, 2) health care use, 3) total health care costs. * Mental Health: examining the effects of marital status and the presence of depression. One of the really interesting things I came across, in preparing this lecture was The Longevity Project. It was initiated by Louis Terman in 1921, and carried forward by Howard Friedman and Leslie Martin. I encourage everyone to read it. Terman tracked 1500 boys and girls, aged 10 to 12. He interviewed them and their families, both growing up, as well into adulthood, later in life, and even after their deaths. Extensive interviews and questionnaires inquiring into so many aspects of life. These folks were followed through education, career, relationships, marriage, sexuality and even included assessment of death certificates. Themes that were examined included: *What type of disposition do you have? Are you cheerful and optimistic? Are you prudent, persistent, and planful? Are you a pessimistic bleak- brooder? Who do you think tended to have the most numbers for longevity? Should I tell you, or would you like to read the book. Ok. I’ll tell you! -The prudent planners did the best! Perhaps not what you might have thought, but the cheerful optimists tended to be less disciplined and focused; less goal oriented; more career problems; less relationship stability; perhaps more narcissistic; smoked more, drank more. The prudent planners tended to set up better lives; more goal oriented; better careers, better organized home lives, more stable families... also the prudent planners were not necessarily prudish. Many of them acknowledged great closeness and love and the enjoyment of wholesome sex as part of their life experience. * What about job stress? Well, there are different types of stress in all categories of life. Is it just a job, clocking in from 8 to 5, not enjoying what you do? Perhaps working for a boss, or others who are disrespectful, difficult, abusive... all grinding away at your sense of being trapped, depressed, very deep rotting stress. OR, do you have a career that challenges and fulfills you, gives you purpose and adds to your identity: a different type of stress! You still may work hard, be up all night, have deadlines, have difficult tasks, etc. but this may be more of life nurturing stress. * What about marriage, which I discussed earlier? Is it a really good marriage, an okay marriage, or a bad marriage? On the one side is the nurturing of the soul and on the other, is the grinding down of the soul. * What about sex? How well mated are you and your spouse emotionally and sexually? Score: "very badly" to "no two could be more perfectly mated". Don't forget this was a longitudinal study from the early to late 20th century: most of it before birth control, the sexual revolution, and civil rights. * What about exercise? Again this was written before the study, science, and commitment of exercise and physical fitness. Interestingly, the most lucky people in terms of longevity were not big exercisers. They tended not to jog, go to the gym, obsess about the number of miles, at what speed, intensity, frequency etc. They tended to be active, enjoying what they were doing: Walking, hiking, swimming, gardening, dancing, finding pleasure with others, and with hobbies that kept their bodies moving. Finally, though many people do well at being alone, and are not lonely, those who are lonely, either by being alone, or as well, with someone in an unhappy relationship, tend to be the ones who suffer more. A bleak existential philosopher named Anatole France, (he's French) said: "It is not customary to love what one has." Pretty sad statement, don't you think? Another statement about relationships-that to me is more pertinent-as stated by psychologist , Michael Kogutek: " If you're not working on it, it's not working!" Another psychologist, Helen Fisher, a couples’ therapist, gave this advice in her book "Why We Love" (2004): * Commit. Listen "actively" to your partner. Ask questions. Give answers. APPRECIATE. * Stay attractive. Keep growing intellectually. * Include him/her. Give him/her privacy. Be honest and trustworthy. * Tell your mate what you need. * Accept his/her shortcomings. Mind your manners. * Exercise your sense of humor. * Respect him. Respect her. Compromise. Argue constructively. * Don't assume the relationship will last forever. Build it one day at a time... My wife and I have a philosophy: Never give up and remember there is no moving forward in a relationship by going backward. Be happy, be well, and don’t let your life or your relationships become stagnant. Step out of your comfort zone and discover something new! (except zip-lining. I won’t do zip-lining!) This concludes the 3 Part essay on "The Not so Simple Tidbits to a Healthy Lifestyle". Yes, there are many resources to go to. There are many resources to go to that might be helpful, but I also wanted to convey that maintaining a healthy lifestyle is way more complicated than instructional reading. I hope you have enjoyed this series as much as I have enjoyed presenting it!  In part 1, I addressed the bleak stuff that humans have to deal with to varying degrees, so let’s now talk about nutrition and exercise. WHAT CAN WE DO TO DO BETTER? A statement taken from the National Institute of Health (NHLBI): " Diet, weight control, and increased physical activity are the first steps in the prevention and treatment of coronary artery disease." This is fundamental. WHERE DO MOST OF US LIVE WITH FOOD IN AMERICA? We have a higher intake of red meat, processed meat, refined grains, sweets and desserts, French fries, high-fat dairy products: I know, I know- All the Good Stuff! WHERE SHOULD WE BE? Higher intake of vegetables, fruits, legumes, whole grains, fish, poultry: (Yuck!) The American Heart Association recommended in 2006 Diet and Lifestyle Recommendations for Cardio Vascular Risk Reduction: Consume an overall healthy diet rich in fruits, vegetables, whole grain, high- fiber foods and include fish at least 2X/ week. Aim for: - A healthy body weight - Recommended levels of LDL, HDL, and Triglycerides - A normal blood pressure - A normal blood glucose level DO THESE THINGS!:
Additionally, eat a higher content of MUFAs. (Mono Unsaturated Fatty Acids- namely Omega's! By doing so, you will promote better lipid (cholesterol) levels, improve blood pressure, improve glucose levels and insulin sensitivity. If you don't have documented coronary artery disease, eat a variety of (preferably oily) fish at least twice a week. Increase oils and foods rich in alpha- linolenic acid (flaxseed, canola, soybean oils; flaxseeds and walnuts). If you do have documented coronary disease, consume about 1 to 2 grams of EPA +DHA per day. (These are the 2 specific omega 3's). If your triglycerides are very high (200 or greater) 2 to 4 grams of EPA and DHA are recommended. The types of fish with the highest levels of EPA +DHA (over 800 mg / 3 oz serving) are:
WHAT ABOUT ALCOHOL? One drink a day improves coronary risk, vs. teetotalers, though increased amount of alcohol is associated with higher mortality risk from numerous causes. There is no difference between red and white wine statistically, though red wine has resveratrol which may have benefits to the integrity of the arterial wall. Alcohol In moderate amount has beneficial effects to lipid metabolism and increases HDL, and lessens clot risk. As a rule of thumb, women are " allowed" one to 1-1/2 drinks a day, and men, up to 2 drinks a day, meaning one drink equals 12 oz beer, 5 oz wine, 1-1/2 oz (shot glass) 80 proof spirits. WHAT ABOUT PHYSICAL ACTIVITY? 26% of adults in the USA report being physically active (>30 minutes) on most days of the week. When physical activity was measured by a device that detects movement, only 3 to 5% of adults obtained > 30 minutes of moderate or greater intensity 5 days a week! Over 40% of adults report no leisure time physical activity. The recommended level of physical activity for general health is 150 minutes/ week which is 30 minutes / day X 5 days/ week. (20 to 30,000 steps / week) For weight loss, it's 250 to 300 minutes / week which is > 60 minutes / day, 5 days a week or more. (40 to 60,000 steps/ week. Help in putting together an exercise program is very helpful, and assessed around Frequency, Intensity, Time ( duration)- FIT Lifestyle activities are also very beneficial if you are not directly into exercise per se, such as stair climbing, yoga, walking, hiking, gardening, dancing, etc. Simply put, you want to do a certain amount of aerobic activity on a daily basis, and certainly 4 to 5 times a week. The formula to apply is 220 minus your age. 90% of that is your aerobic threshold. You don't have to get there, nor do you need to exceed that. For most people not a great idea to exceed that. Most aerobic conditioning is in the 75 to 90% range. BUT, 65 to 75% will allow for caloric reduction and “fat burning”.
When I address these issues to patients, I always encourage comfortable walking for several minutes at the beginning and at the end, and in between, do a power walk for as long as you comfortably can. Note how long it lasted until you wish to slow down, and repeat the same daily for two weeks. After two weeks add another 2 to 3 minutes to the power walk per week, and gradually, your aerobic capacity, and conditioning can't help but improve. The other aspects of exercise I address, are stretching for continued flexibility, some weight or resistance work to develop muscle strength and tone, and balance. With aging, balance gets compromised and you need to work on it! The tough part is that it takes a lot of exercise for calorie reduction, versus the amount of food to add caloric gain. For example, 40 minutes of intense aerobic exercise is worth about 400 to 500 caloric loss, which is about one piece of chocolate cake or a slice of pizza! Resistance training (free weights or machines) does not promote clinically significant weight loss, although it may increase muscle mass which may increase 24 hour energy expenditure. Energy intake ( food) is influenced by many environmental factors: the composition and density of foods, the volume of foods, portion size, visual cues, prior intake patterns, variety, and setting ( alone vs. group, other stimuli, etc.) meal replacement programs (protein shakes for example) may help drop weight by 5 to 10% if used daily for one or two meals. Though low carb diets are often helpful in dropping weight, they tend to rebound back up to initial levels when stopped. The "diet" that I recommend in my practice which is advised by the National Lipid Association, and now by the American Heart Association, and American College of Cardiology, is the Mediterranean Diet, which is much more an approach to nutrition rather than a diet. This tends to lower weight more gradually and keep it off and also has most of the heart healthy benefits that have been previously discussed in this essay. Also be aware of the GLYCEMIC INDEX, which is a measurement of the glucose level of certain vegetables and fruits. You can look these up in Google, but foods such as white rice, potatoes, corn flakes and other cereals, bananas, carrots, white bread, white spaghetti are all on the higher side. Here are a few secrets of people with successful long term weight management: * 78% of people eat breakfast every day * 75% weigh themselves at least once a week * 62% watch less than 10 hours of TV/ week * 90% exercise, on average about 1 hour/ day Here are some tips that help you to lose weight: * Keep a journal: it helps you create patterns and reinforces the mission. * Daily exercise: burns calories and improves overall health * Protein at every meal: maintains muscle mass and higher satiety quality * Regular eating patterns: Minimizes grazing and binging * Take it slowly: healthy patterns develop over time * Meal replacements (1 or 2/ day): facilitates long term weight loss * Find a partner or attend a support group: this helps to maintain new lifestyle habits * Eat a Rainbow : Fruits and vegetables provide variety and fill you up. This concludes Part 2 of Not So Simple Tidbits for a Healthier Lifestyle. In Part 3, I'm going to discuss some other areas of importance attributed to helping you live a longer, healthier, and happier life. Until then, get out and move your body and follow the above dietary guidelines! |
AuthorBrian Chesnie M.D. Categories
All
Archives
August 2019
|
||||||

 RSS Feed
RSS Feed